Extreme heat health risks in ultra-rural communities
When climate, health, and poverty collide

Farmers struggle with drought and food shortages due to climate change.
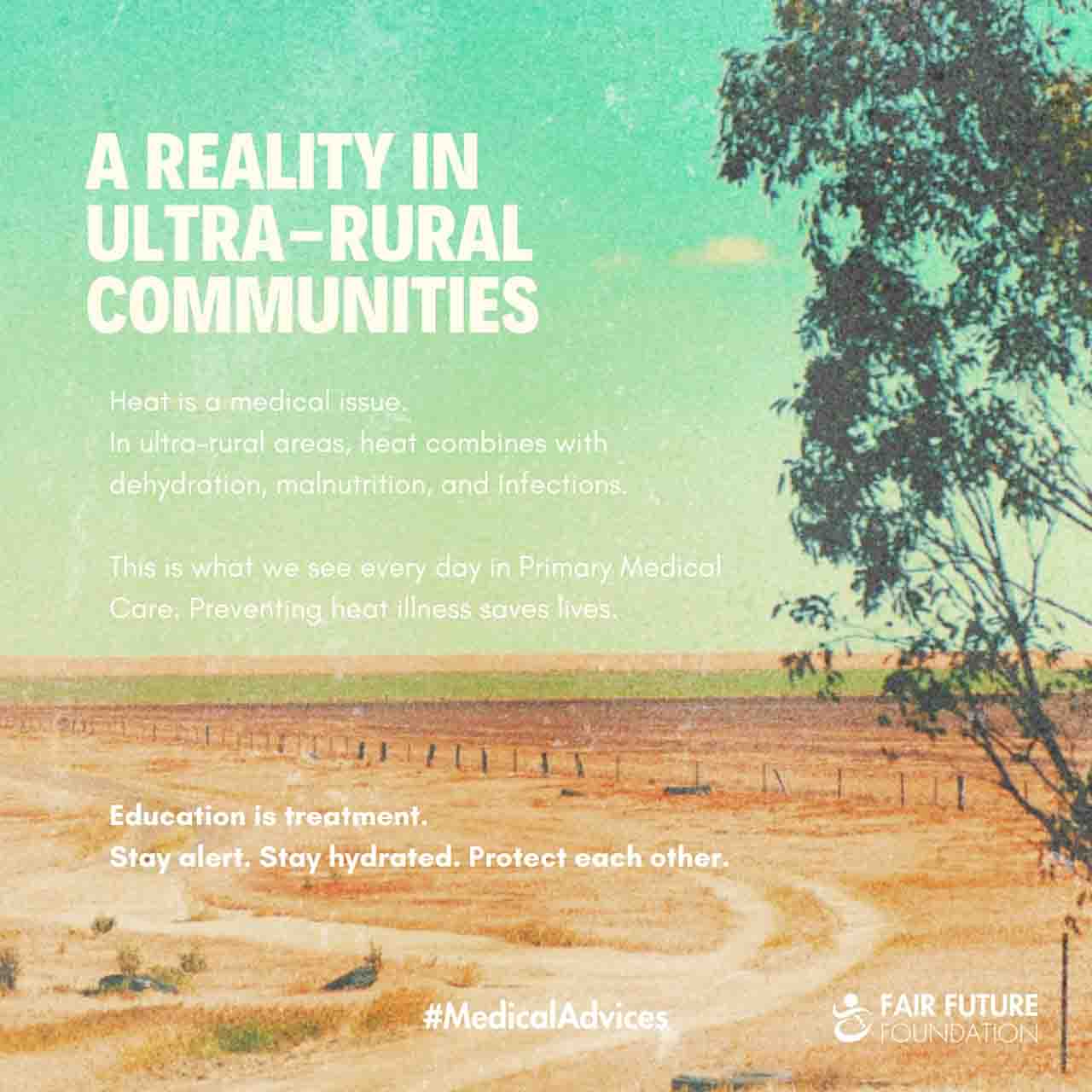
Medical advice on recognising and preventing heat illness in ultra-rural communities affected by climate change.
Extreme heat health risks transcend theoretical discussions and manifest with alarming reality in ultra-rural communities. In the villages where Fair Future and Kawan Baik Indonesia work every day, heat interacts deleteriously with dehydration, malnutrition, infections, and arduous physical labour. Within the domain of Primary Medical Care, we approach heat illnesses as medical emergencies that are preventable through straightforward, life-saving interventions.
In ultra-rural regions of Indonesia, soaring temperatures inflict severe stress on vulnerable bodies. As core body temperature rises, mechanisms to cool the body falter. Rapid loss of water and electrolytes can precipitate a dangerous drop in blood pressure, compromising organ function. Those most susceptible include children, the elderly, pregnant women, and manual workers—especially in areas where access to clean water and adequate shade is limited.
Climate change exacerbates these health risks by extending dry seasons, spiking temperatures, and making rainfall erratic. These climatic changes intensify dehydration, exacerbate malnutrition, and aggravate infectious diseases, leading to a rapid deterioration of health conditions and converting minor illnesses into critical emergencies.
Early recognition of heat-related danger is vital to saving lives. Symptoms such as headache, dizziness, extreme fatigue, nausea, confusion, and hot, dry skin signal the body’s distress. Prompt action is essential and includes regular hydration, ceasing physical activity, seeking shade for rest, cooling the body with water, minimising exertion during peak heat, and ensuring children are never left alone in hot environments.
Education serves as an intervention in itself. The “medical advices” we impart is garnered from our on-the-ground experiences with these communities. Once shared, comprehended, and perpetually echoed, these preventive strategies significantly minimise suffering and avert fatalities. In our progressively warming planet, safeguarding health is rooted in informed awareness and a shared sense of responsibility.
Today, the 23rd of December 2025 – Alex Wettstein
In Short – When heat becomes a diagnosis
In ultra-rural villages, heat illness rarely appears alone. It amplifies infections, weakens immunity, and accelerates dehydration. What looks like fatigue is often a medical emergency. Teaching people to recognise early signs and act immediately saves more lives than treatment alone.
About this topic on our Instagram page
List of Related Organisations with Hyperlinks
- World Health Organisation: Describes how extreme heat impacts human health and increases mortality worldwide.
- UNICEF: Explains why children are particularly vulnerable to heat stress and dehydration.
- Médecins Sans Frontières: Reports on heat, dehydration, and medical emergencies in low-resource settings.
- International Federation of Red Cross and Red Crescent Societies: Heatwave preparedness and community prevention strategies.
- Centers for Disease Control and Prevention: Medical signs, symptoms, and prevention of heat illness.
- UN Environment Programme: Links climate change to increasing health risks in vulnerable populations.