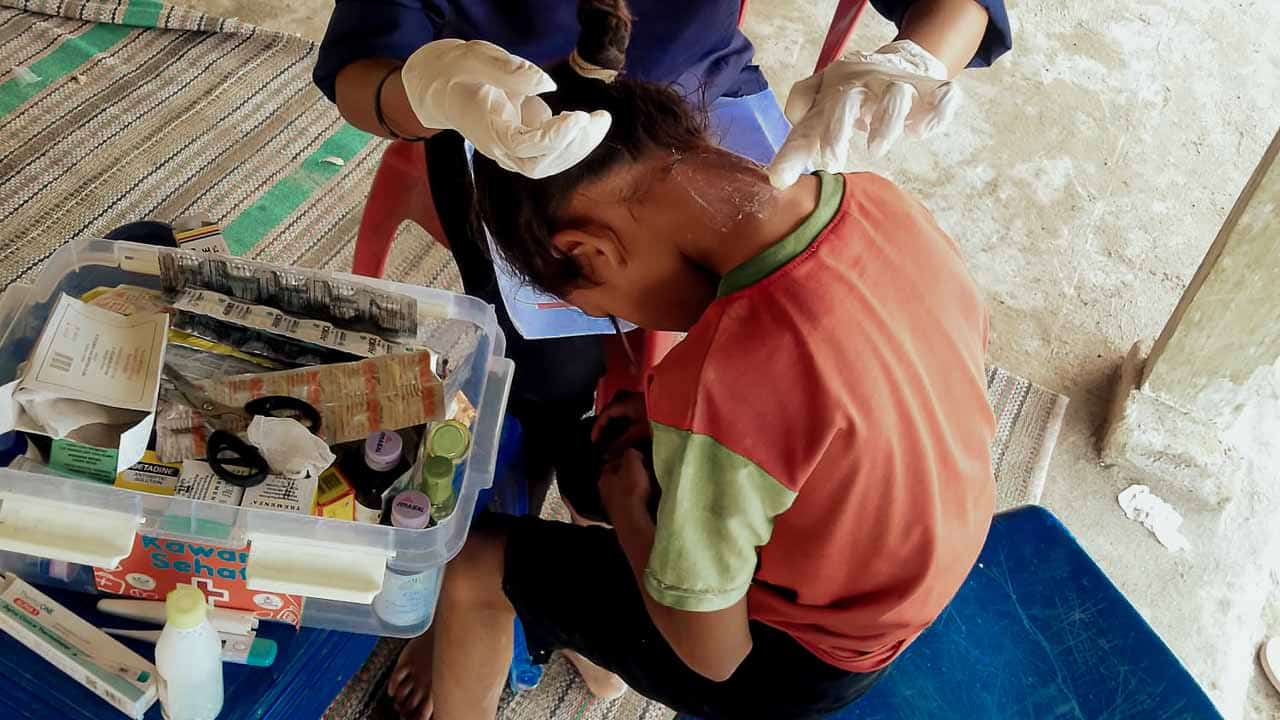
Through the Primary Medical Care program, Kawan Sehat health workers provide treatment for fevers, wounds, and malaria in villages lacking access to doctors. They carry essential medicines, adhere to established medical protocols, and refer emergency cases promptly to prevent delays in care.
Donate
Support Care
Programs
All projects
Quick News
Field updates
Stories
Field stories
No Access to Rural Healthcare | Life Without Medical Care
Since 2006, Fair Future has been on a mission to create lasting change in the most vulnerable and remote regions of Southeast Asia. Through collective action, we’ve built hospitals, provided clean water, and delivered essential medical services, turning seismic challenges into transformative opportunities for thousands.
No Access to Healthcare in Rural Areas
When distance replaces diagnosis

In their house in Lahiru, Sarlota and Yosef explain how to take the medicines to a father and his children.
What Happens When There Is No Access to Healthcare
In many rural regions, lack of access to healthcare is not a policy issue or a theoretical gap. It is a daily, concrete reality. Rural healthcare often does not exist at all, leaving people to live with illness without medical consultations, accurate diagnosis, effective treatment, or follow-up care. This lack of healthcare means that pain, fever, infection, and pregnancy complications unfold without medical guidance, protection, or timely intervention.
This void in healthcare directly shapes how diseases progress, how families cope, and how lives are lost. In ultra-rural areas where roads are absent, electricity is unreliable, and clean water is scarce, healthcare services are often nonexistent.
Rural healthcare in these settings is not weak or delayed. It is missing entirely. The situation is not defined by crises but by continuous silence, structural delays, and preventable suffering that accumulates over time.
To understand what life without healthcare truly entails, one must examine its medical, structural, and human consequences together. These realities are not theoretical. The Fair Future Foundation encounters them every day on the ground, working within communities where access to care remains a defining condition of life.
©Alex Wettstein – Fair Future Foundation, the 6th of January 2026/aw
Absence of medical infrastructure
In ultra-rural regions of Southeast Asia, particularly in East Sumba, eastern Indonesia, a lack of access to healthcare defines daily life. Many villages are several hours from the nearest health facility, often without roads, transport, or financial means. There are no clinics to consult, no trained medical staff, no diagnostic tools, and no essential medicines. Healthcare does not start late. It does not start at all.
Living with disease
Families manage illness at home without diagnosis or guidance. Fever, wounds, pain, or pregnancy complications are observed but not medically assessed. The lack of healthcare leaves people alone in the face of disease, relying on intuition rather than medicine.
An empty system
In these settings, rural healthcare is not fragile or limited. It is absent, and this absence determines survival.
From symptoms to complications
Clinically, the consequences of this absence are predictable. Minor wounds become infected due to a lack of cleaning, antibiotics, and follow-up. Fever is often considered benign until it evolves into severe malaria, anaemia, or sepsis. Diarrheal diseases lead to dehydration and death, especially in children.
No prevention, no continuity
There is no early diagnosis, no preventive care, and no continuity of treatment. Chronic conditions remain unmanaged. Pregnant women give birth without antenatal care, skilled assistance, or referral options. Care begins only when complications are advanced.
Mortality by default
In ultra-rural contexts, mortality increases not because diseases are complex, but because basic medical care is missing.
Geography as a clinical factor
In East Sumba, geography directly shapes health outcomes. Villages are isolated, sometimes cut off for weeks during the rainy season. Distance translates into delayed care, missed diagnoses, and untreated conditions. From a medical perspective, distance itself becomes a risk factor.
Infrastructure and exposure
The absence of electricity, clean water, and sanitation increases exposure to infectious diseases. Malaria, skin infections, gastrointestinal illnesses, and respiratory diseases follow recurring patterns. Without clean water, prevention is impossible. Without electricity, storage and diagnostics are limited.
Systemic exclusion
Health systems stop where logistics become complex. Beyond that point, populations are structurally excluded from care. Medicine exists, but it does not reach them.
A daily medical presence
This is the reality Fair Future Foundation faces every day. Through the Primary Medical Care programme, trained Kawan Sehat health agents provide frontline medical care directly in ultra-rural villages. Every day, new cases are treated. Every few hours, questions arrive via the Kawan Sehat application about wounds, infections, fever, antibiotic use, or follow-up decisions.
Clinical supervision
Medical teams review cases, analyse images, and adjust treatments in real time. More than 1,000 patients are treated every month, restoring continuity where no system exists.
Care that saves lives
Supported by Swiss medical expertise, protocols are adapted to field realities. Primary Medical Care fills the gap where healthcare is absent.
What already exists
The future of healthcare in ultra-rural regions does not start from nothing. It starts from what is already in place. The Primary Medical Care program has shown that with limited means, structured protocols, and trained local health agents, lives can be saved every day. Treating more than 1,000 patients each month in East Sumba proves that even a basic medical presence changes outcomes.
What must continue
Continuity is essential. Healthcare only works when it is stable, trusted, and present over time. Training, supervision, medical supplies, access to clean water, and prevention must remain constant. Interruptions cost lives. The challenge is not innovation, but durability. Keeping Primary Medical Care active means protecting families from preventable complications, month after month.
A realistic medical vision
Fair Future Foundation’s vision is simple and grounded. Continue where we are. Strengthen what works. Expand carefully, without losing quality. With more means, more villages could be reached. Without excess, without slogans. Just sustained medical presence where healthcare is still absent.
Care Where Healthcare Does Not Exist
Key facts on healthcare access
- Nearly half of the world’s population still lacks access to essential health services, mainly in rural and remote areas.
- Treatable conditions such as malaria, infections, diarrhoea, and pregnancy complications remain leading causes of death where care is absent.
- Communities without healthcare infrastructure are the first to suffer from climate stress, epidemics, and preventable mortality.

Primary Medical Care
Kawan Sehat health agents walk hours to treat fever, malaria, injuries and dehydration in villages without clinics, where climate shocks hit first.
Water Connections
Ferro cement reservoirs and village water networks secure clean litres during longer droughts and after floods, cutting diarrhoea and kidney problems.
Kawan Against Malaria
Prevention, early diagnosis and treatment of malaria in areas where changing rains and temperatures create new mosquito patterns and higher risks.
Solar lights for families
Solar lamps for homes and schools reduce injuries at night, improve study conditions and cut toxic fumes when electricity is absent or unreliable.