Umalulu malaria baseline guides nets, IRS, WASH, and access improvements to reduce transmission.
Door-to-door data from 269 households informs practical village-level action.

A typical household in Umalulu, where poor housing, open defecation, and standing water increase the risk of malaria. This image was taken during the 2025 baseline survey.
Umalulu Malaria Baseline: Turning Door-to-Door Evidence into Action
Summary
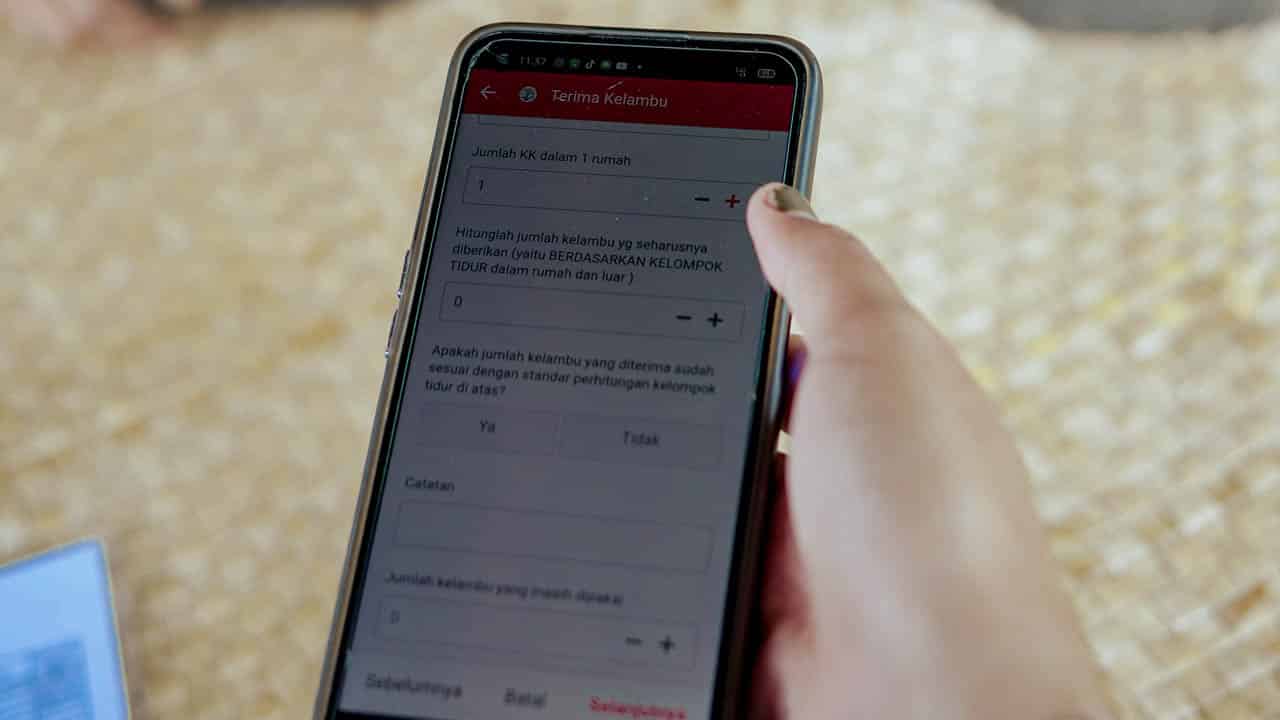
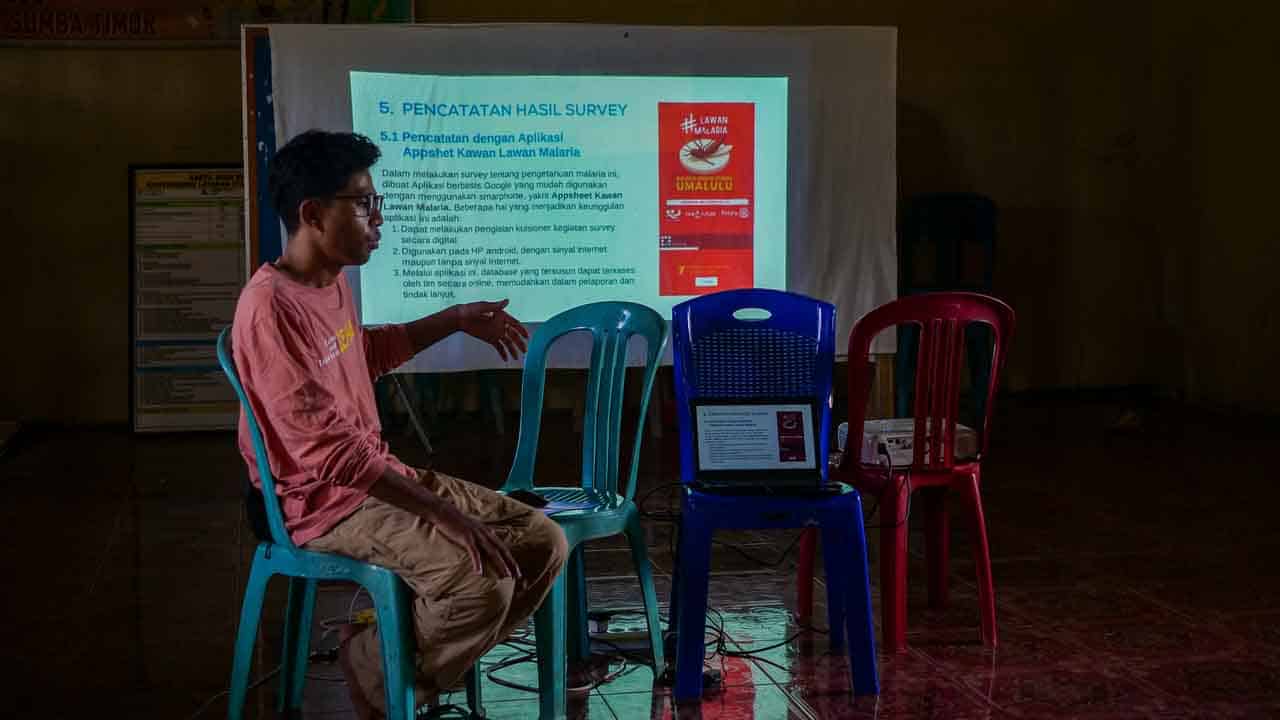
From March to the end of July 2025, Fair Future and local partners conducted a door-to-door baseline in Umalulu, East Sumba. Trained village cadres and Puskesmas staff, equipped with an offline mobile app, visited 269 households and completed 460 interviews, documenting housing, sanitation, behaviours, care-seeking, diagnostics, and exposure patterns. This work establishes the first household-level baseline for the area and provides a concrete roadmap to reduce malaria risk.
Why this baseline matters
Umalulu is a recurrent early detection point in East Sumba, with transmission peaking during the August–November dry-to-wet transition. By replacing assumptions with primary, door-to-door data gathered by local teams, the study sets a defensible starting point for targeted control and for measuring progress over time.
Methods in brief
- Study type: cross-sectional household–environment survey + knowledge/experience module.
- Team: village cadres and Puskesmas staff after a focused refresher (epidemiology, vector ecology, interviewing, app use).
- Data capture: offline-first mobile application with later synchronisation and geo-tagged photos.
- Definitions: Net ownership is household-level (≥1 LLIN); coverage is sleeping-space level (beds/mats/hammocks). Denominators vary by sub-sample.
Key findings to act on
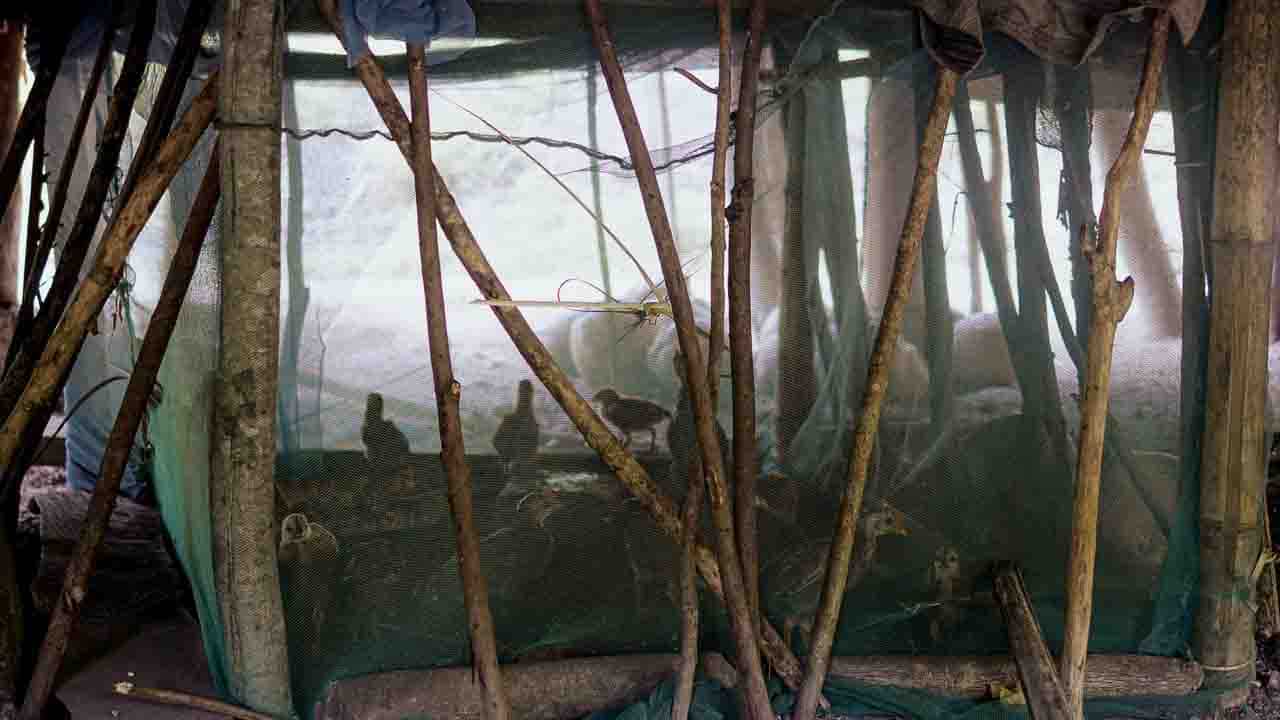
- Uneven vector control. Only 1.1% of households reported any indoor residual spraying (IRS). Net protection is better but incomplete: 68% of sleeping spaces are fully covered, 27% partially, and 4% are unprotected; >92% of nets are over one year old.
- Sanitation & water. 56.9% of households still practise open defecation; limited septic containment creates grey-water pools and larval habitats.
- Diagnostics close to homes. RDTs predominate; 68% of tests were performed at home by village cadres—underscoring the centrality of community-based case finding.
- Access is insured but distant. 93.7% report KIS/BPJS coverage, yet more than half live >5 km from care and many require 15–30 minutes (or more) of travel—making decentralised testing/treatment essential.
- Partial knowledge. About 77% knew that Anopheles bites transmit malaria, but roughly 68% could not name common breeding sites—helping explain persistent exposure despite awareness campaigns.
What changes next: our action roadmap
- Maintain & replace LLINs — repair when possible and target partially covered sleeping spaces ahead of Aug–Nov.
- Build IRS capacity — train spray teams, provision pumps/insecticide, and schedule seasonal rounds.
- WASH + source reduction — expand latrines/septic systems and run community clean-ups to eliminate breeding sites.
- Maintain close diagnostics — ensure uninterrupted RDT stocks and cadre refresher training to sustain home-based testing.
- Reduce access frictions — motorbike outreach; solar lighting/micro-grids to reduce night-time exposure; targeted transport support for remote hamlets.
Data governance & ethics
The digital file on the Fair Future server is the only controlled copy; printed or forwarded files become uncontrolled once a new version is issued. An anonymised dataset and the financial report are available on request under a simple data-use agreement.
Download the reports
PDF – Scientific Report (IMRaD format) | This version, structured for academic and policy use, presents methods, results, discussion, and limitations in a concise scientific format (4.5mb).
PDF – Fair Future Foundation FULL Report | A comprehensive version incorporating social impact, medical findings, and an action roadmap for communities, local authorities, and partners (34mb).
PDF – ARAM Technical & Financial Report | Prepared for Rotarians Against Malaria (ARAM), this edition includes the baseline study results along with financial reporting and supporting documents (0.5 mb).
Today, the 20th of August 2025 – Alex Wettstein
In Brief — High-Resolution Baseline, Actionable Epidemiology
A door-to-door cross-sectional survey (269 households; 460 interviews; 693 sleeping spaces) produced a high-resolution risk profile for Umalulu. Vector control is inconsistent (68% spaces fully net-protected; 27% partial; 4% none; >92% nets >1 year), with IRS 1.1%. Sanitation gaps persist (56.9% open defecation), and night-time activity coincides with the Aug–Nov transmission window. Diagnostics are decentralised (RDT-led; 68% tests at home), yet distance to facilities (>5 km for many) sustains access friction despite 93.7% insurance coverage. Geo-tagged, offline-captured observations isolate levers: LLIN replacement/repair, seasonal IRS, household WASH & larval-source reduction, and uninterrupted community testing.
From Home to Data – Building a Malaria Baseline in Umalulu
List of Related Organisations with Hyperlinks
- WHO Global Malaria Programme: Technical guidance for malaria control and elimination worldwide.
- RBM Partnership to End Malaria: Global coalition accelerating coordinated action against malaria.
- UNICEF Indonesia: Child health, WASH, and education programmes in Indonesia’s rural provinces.
- The Global Fund: Financing for malaria, HIV, and TB programmes with community-based delivery.
- PATH: Innovation and implementation support for diagnostics, vector control, and primary care.
- Malaria Consortium: Operational research and delivery of prevention and case management.
- Clinton Health Access Initiative: Market shaping and programme support for malaria commodities.
- Indonesian Ministry of Health: National policy, surveillance, and primary-care strengthening.
- East Sumba District Health Office: District surveillance, Puskesmas oversight, and vector-control operations.