Incidence of tuberculosis in Indonesia
The World Health Organization (WHO) has designated Indonesia a “high burden country” for tuberculosis.
There are 22 high burden countries worldwide, and together they account for about 80 percent of the world’s tuberculosis infections. Expatriates or frequent travelers who spend a significant amount of time in a high-burden country may benefit from TB screening. Some countries may recommend that infants and children have a BCG vaccination.
In Indonesia, there are roughly 500,000 new cases of TB annually and 175,000 attributable deaths. Tuberculosis is the second major killer of adults after cardiovascular disease and the deadliest pathogen out of all communicable diseases.
In global terms, there are one billion people infected with tuberculosis at any one time. Eight million new cases are reported annually with three million attributable deaths. However, despite these grim figures and without the influence of consistent treatment and immunization, its incidence is not as high as it was in the 20th century. The problem now is that with inadequate and inconsistent treatment regimes, a pool of persistent sputum-positive cases is being created.
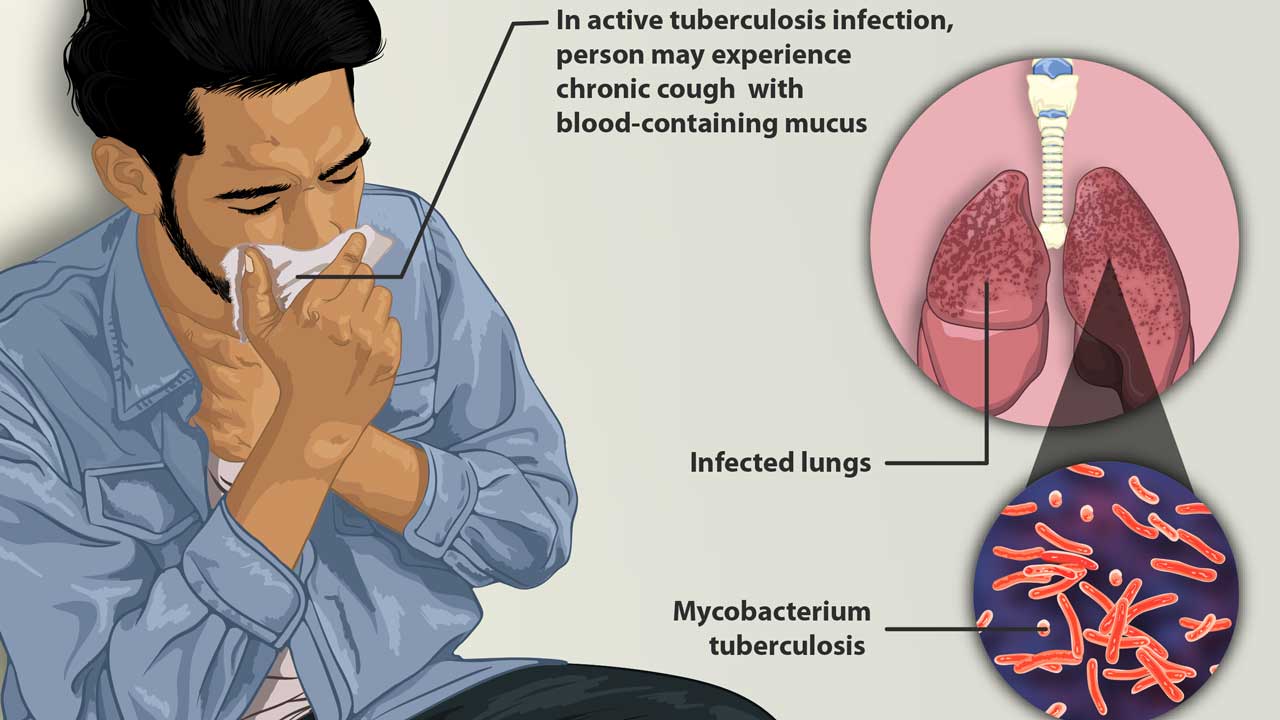
Poverty facilitates the transmission of “Mycobacterium tuberculosis”. It is easier to catch TB if you live in poor, dirty, damp, dark or dusty conditions. Tuberculosis bacteria can live longer in damp, dusty rooms where there is no fresh air. Prolonged delay in diagnosis and increased vulnerability due to malnutrition and/or HIV infection. If it is dark, bacteria cannot be killed by sunlight. Poor living conditions and overcrowding increase the risk of tuberculosis.
Tuberculosis deaths rise for the first time in more than a decade due to the COVID-19 pandemic
The COVID-19 pandemic has reversed years of global progress made in the fight against tuberculosis and, for the first time in more than a decade, deaths from tuberculosis (TB) have increased in 2021.
Indeed there are far fewer people diagnosed, treated, or receiving preventive treatment against the disease compared to 2019, and overall spending on essential TB services decreased.
Disruptions in access to TB services and reduced resources. In many countries, human, financial, and other resources have been reallocated from TB to COVID-19 response, limiting the availability of essential services.
Symptoms and Diagnosis of tuberculosis
Active TB causes a variety of symptoms that are sometimes vague, but often include cough, fever, night sweats, unintended weight loss, and lethargy. Latent (inactive) TB causes no symptoms. Most strains of TB can be treated with antibiotics. Up to four different types of antibiotics may be used together to treat a patient. If left untreated, active TB can be life-threatening.
At the local level, diagnosis is best achieved through microscopic detection of bacillus in a sputum smear. Culturing bacillus is expensive and impractical as it takes 6 weeks for results, and x-rays can be misleading. The most widely used test for diagnosing active TB in low- and middle-income countries relies on examining a patient’s phlegm under a microscope.
This method, developed almost 140 years ago, detects less than half of all TB cases and largely fails to detect the disease in children and people co-infected with HIV – who usually cannot. produce the necessary sputum – and those that have drug resistance. forms of tuberculosis.
One diagnostic test, Xpert MTB/RIF*, cannot be used in many resource-poor settings, such as the rural areas where Fair Future is active.
It has been recognized that males in the 25 to 34-year old age group are the most common transmitters of the TB bacillus. An infectious case will typically infect up to ten other people in a year. In case-finding, the general rule is that anyone who has had a cough for more than 3 weeks should have a sputum smear. Crowded dark places are ideal areas for the spread of TB, as direct sunlight will kill the bacillus in a few minutes but it can live in dark and dusty areas for up to 20 years.
*The Xpert MTB/RIF is a cartridge-based nucleic acid amplification test (NAAT) for simultaneous rapid tuberculosis diagnosis and rapid antibiotic sensitivity test. It is an automated diagnostic test that can identify Mycobacterium tuberculosis (MTB) DNA and resistance to Rifampicin© (RIF). It was co-developed by the laboratory of Professor David Alland at the University of Medicine and Dentistry of New Jersey (UMDNJ)
Treatment of tuberculosis
No matter the treatment regime used, the following basic rules must be observed:
- Any drug intake must be supervised.
- Drug intake must continue until otherwise directed, which may be many months.
- There needs to be an uninterrupted drug supply to prevent emergent drug resistance.
When patients are resistant to the two most potent first-line antibiotics (rifampicin and isoniazid), they are considered to have multidrug-resistant tuberculosis (MDR-TB*). Treatment is long and arduous, with the drugs having many potential side effects, including psychosis and deafness. People can take up to 20 pills a day for two years – only to have a cure rate of just under half. Extensively drug-resistant tuberculosis (XDR-TB) occurs when a patient is resistant to second-line drugs. Only a third of people with XDR-TB are cured.
It is essential that a patient completes all of their treatment, even when they begin to feel better. incomplete treatment can lead to the development of drug resistance. Decentralizing treatment by having people care at home can help them adhere to treatment and overcome barriers they may face.
Most drugs to treat tuberculosis are old and toxic. But over the past decade, Bedaquiline©*, Delamanid© and Pretomanid©, three new tuberculosis drugs – the first in half a century – have been developed, giving patients hope and options for treatment providers.
But making these drugs available to patients who desperately need them has been painfully slow.
To date, one in eight people with drug-resistant tuberculosis who could have benefited from the new life-saving drugs Bedaquiline© and Delamanid© have been treated with them.
Prevention of tuberculosis
Travellers and expatriates may be able to reduce their chance of contracting TB by limiting the amount of time they spend in crowded places. Avoiding people who are coughing also minimizes risk. If you live in an area with higher rates of TB infection, consider screening local staff who live with you – especially if you have young children in your household.
The BCG vaccine has been used for many years and is usually given to infants in the first month of life. Studies have shown conflicting results, ranging from limited usefulness to 14 years of protection. However, it only provides protection against serious diseases.
Countries such as Canada and the USA have preferred to concentrate their preventative efforts by monitoring the spread of the disease and treating those who test positive, rather than immunizing the whole population. They feel that a positive test fails to differentiate those who have been immunized from those who actually have the disease and that the vaccine is ineffective and complicates diagnosis which takes many weeks to begin with.
European authorities believe that even the partial protection provided by the BCG vaccine is worth the increased diagnosis difficulty, and they also believe that repeated Tine testing will cause a false-positive reaction after a number of tests. This is caused by a response to the inoculation with reactive parts of the organism in the previous tests.
MDR-TB: The bacteria that cause tuberculosis (TB) can develop resistance to the antimicrobial drugs used to cure the disease. Multidrug-resistant TB (MDR-TB) is TB that does not respond to at least isoniazid and rifampicin, the 2 most powerful anti-TB drugs;
Bedaquiline: Sold under the brand name Sirturo, is a medication used to treat active tuberculosis. Specifically, it is used to treat multi-drug-resistant tuberculosis (MDR-TB) along with other medications for tuberculosis. It is used by mouth;
Delamanid: Sold under the brand name Deltyba©, is a medication used to treat tuberculosis. Specifically, it is used, along with other antituberculosis medications, for active multidrug-resistant tuberculosis. It is taken by mouth;
Pretomanid: This is an antibiotic medication used for the treatment of multi-drug-resistant tuberculosis affecting the lungs. It is generally used together with Bedaquiline© and Linezolid©. It is taken by mouth
Differences in urban and rural treatment
Nearly 25% of patients living in rural areas consulted traditional healers before the diagnosis of tuberculosis, which is also the case for other illnesses or injuries. The others, nearly 75%, did not consult doctors or other health professionals. In effect, this leads to continued transmission of TB in villages and communities due to delays in diagnosis and presentation of TB in health facilities at an advanced stage of the disease.
Patients in rural areas have virtually no individual access to anthelmintic drugs. It should be noted that patients from these rural areas also have less or no access to healthcare and health checks. This is valid for the most morbid diseases such as; HIV, COVID, Tuberculosis, Cancer, diabetes…
These differences in TB epidemiology and co-infections underscore the importance of public health interventions such as Fair Future or Kawan Baik do, not only in rural and ultra-peripheral areas of Indonesia, but elsewhere in the world.
Prevention of the spread of infections from a single source
In order to limit the spread of infection in confined spaces and crowded areas such as offices, institutions, and schools, Fair Future observes and recommends that the following minimum precautions should be observed in addition to the medical and possibly radiological screening of the staff :
- Sanitary and washing facilities in accommodation should be clean and cabins should be available for individual ablutions and sleeping;
- There should be a generous supply of clean towels. Soap and warm or hot water should be provided in all sanitary facilities, especially near kitchens and toilets;
- Mess rooms with facilities for covering food and washing hands should be available;
- Paper napkins are preferable to cloth napkins;
- Living and sleeping areas should be constantly inspected for health issues;
Especially in air-conditioned, humid, and confined environments, people with respiratory infections should not go to work when sick without consulting a doctor. Such environments are ideal for the spread of tuberculosis via aerosol droplet transmission;
A system should be in place to report symptoms of throat and chest infections and provide medical supervision of site personnel.
#tuberculosis #covid #tb #hiv #tbc #endtb #aids #coronavirus #cancer #hivawareness #hivaidsawareness #diabetes #worldtuberculosisday #worldtbday #stoptb #healthcare #tuberculosisawareness #hepatitis #diskriminasihiv #d #health #tosstb #itstimetoendtb #healthforall #test #tbcparu #tosstbc #indonesia #tbparu #publichealth #gerdanxietyindonesia #gerdanxiety #anxiety #verstyle #panicattack #maagkronis #gastritis #bottom #dispepsia
Your comment and feedback is invaluable
…to all of us here who are working in the field. You have a role to play, you can bring us your knowledge, it will be greatly appreciated. Thank you so much for your words and your benevolence.