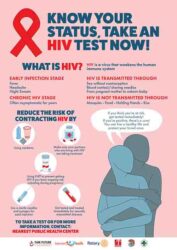
Illness often begins long before someone arrives at the hospital. Our campaigns on smoking, waste management, alcohol, and sexual health display straightforward messages across schools and village walls in local languages. Through simple posters, talks, and games, we help protect thousands of children.
Donate
Support Care
Programs
All projects
Quick News
Field updates
Stories
Field stories
Fair Future Foundation, a Swiss-based non-profit, is an innovative force in global healthcare and social aid.
We work in some of the most remote regions of Southeast Asia, where there are no doctors, no electricity, and often no clean water. For over sixteen years, Fair Future has been on the ground, creating long-term medical and social solutions with the communities who live here.
Through the Primary Medical Care programme, we treat wounds, infections, HIV, malaria, tuberculosis, and chronic illnesses directly in remote villages. With access to clean water, safe reservoirs, and nutritional support, communities can finally prevent disease rather than suffer from it.
Our approach is simple: stay close, listen, understand, and act with science and solidarity. Every action we take aims to strengthen families, improve health, and reduce preventable deaths.
Your support sustains this work. It transforms long days under the sun, muddy roads, and emergency care into measurable change for those who have nowhere else to turn. Alex Wettstein – Fair Future Foundation – Updated in November 2025
Help deliver medical care where no doctors work
Every contribution funds direct care in remote villages. Medicines, wound treatment, diagnostic tests, clean water systems, and solar-powered cold chains to protect vaccines and enable care at night.
Explore our field work and medical reports
Search our articles, field stories, medical updates, and project reports from the ground
Stories from the Field
Real moments from our medical and humanitarian missions in ultra-rural Indonesia. Nothing arranged — just life, as we live it with them.
 ▶
▶
Nov. 2025 | The Day Night Changed
The film The Day Night Changed is now online. It shows how Mbajik School in East Sumba received electricity for the first time after five days of hard work with Smart Energy Tech and the villagers. The final scene shows the first cinema night ever held in Haray.
View the film on YouTube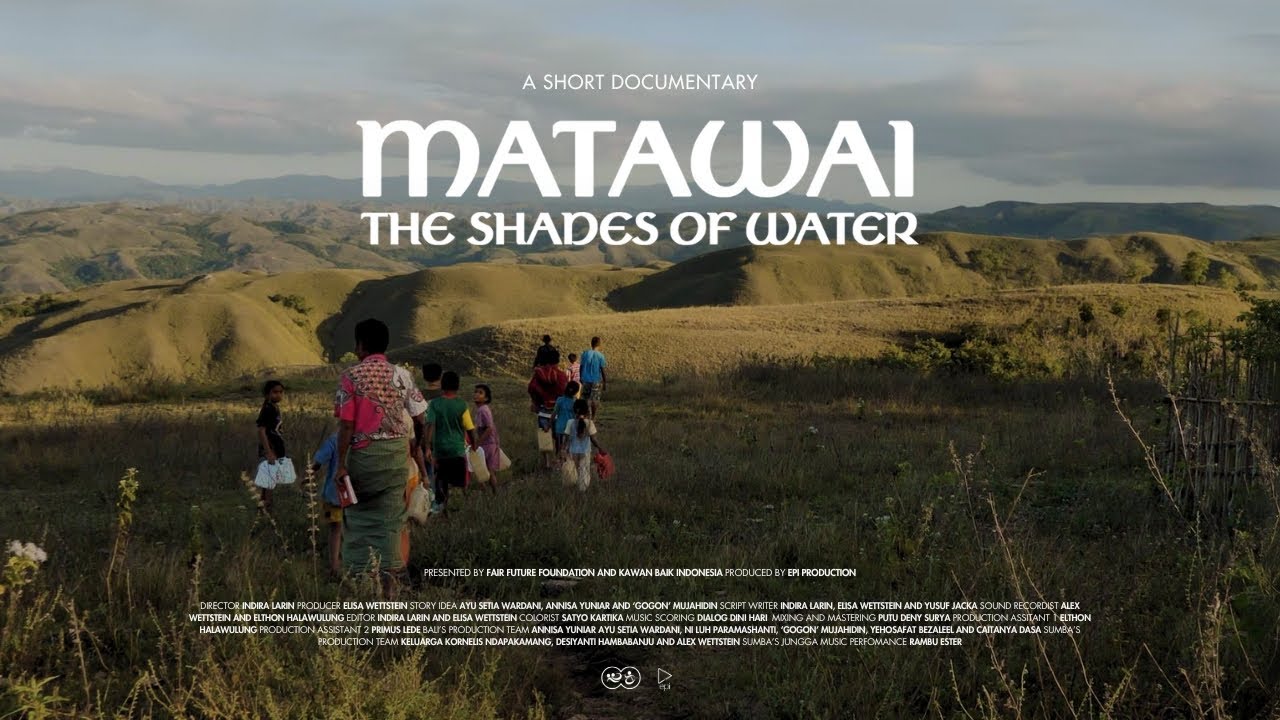 ▶
▶
Matawai, The Shades Of Water
Produced by Fair Future, this 15-minute documentary examines the daily struggle for access to water in the ultra-rural eastern Sumba region. Matawai reveals how the lack of clean water affects women and children, while also highlighting the vital impact of Fair Future's Water Connections programme.
Watch Matawai on YouTubeHow your donations are used?
Fair Future directs 93% of every donated franc to field projects, including medical care, clean water systems, and malaria prevention. Full financial reports are published and audited annually
%
Social and medical actions
%
Fundraising work
%
Field operations and management
WHAT WE ARE DOING NOW
Field stories of wounds treated, clean water built, and families protected
These articles are not reports — they are moments from the field. They show how we care for wound infections, bring clean water to villages, train health agents, and travel days to reach isolated families. This is the reality of our medical work.
Helping ultra-rural families to have a healthier life
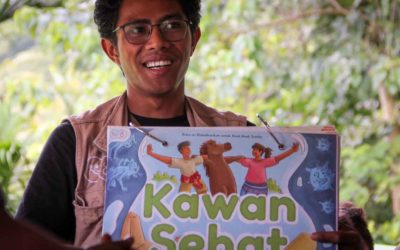
This new "Picture of the Day" features Kawan Ino, one of the Fair Future team members in Sumba (Rumah Kambera Leader), talking to health workers and the village community of Kabanda. To do this, he uses the "Kawan Sehat" book we produced at the end of 2022 for children in these regions. This book is an integral part of the program of access to primary medical care for children in ultra-rural areas.
We spend two days here, and you can read what we have done in Kabanda. This village is genuinely one of the most isolated I have ever seen. Getting it is difficult, even dangerous, at times. No road leads to this village; only extremely steep or steep stony paths allow us to go there. Kawan Ino explains how to have a healthier life thanks to implementing specific things in everyday life. This includes physical and mental health, body and home hygiene, daily habits and women empowerment.
Thanks to the Kawan Sehat program, we see a significant improvement in the health and well-being of rural populations. It is truly heartening to see healthy habits being encouraged and access to health care increasing. It is vital that everyone has access to quality health care, and we are happy that this program allows more people to receive the care they need.
Here, when a person is sick or injured while a woman is due to give birth, one of the only ways for her to receive medical attention is to carry her on people's backs for several hours or even a whole day until the nearest health centre. This person also does not know if he will arrive in time at the medical centre, called "Puskesmas or Pustu", as we have seen on several occasions.
This is why this book is necessary: “Kawan Sehat” is intended for schools and teachers. It's an amazing teaching aid for them, and kids love it. Nothing is done here to give children the means to learn from an early age how to wash themselves, eat healthier, use soap, and learn not to pollute or brush their teeth etc… In the classrooms here in East Sumba, the book“Kawan Sehat” is the only one available for children; there are no others.
Access to clean water is vital for human health
This "Picture of the Day" shows young children's struggles in East Sumba. The jerry cans are heavy and sometimes more prominent than the children themselves. With limited access to drinking water sources, the kids who live there (here in these images in the villages of Kabanda, Mahu, Laindatang, and Tana Mbanas) are forced to walk long distances to fetch water. Water in rivers or wells which are also contaminated. It takes up a lot of their time and puts them at risk of injury or illness by carrying heavy loads of water. Lack of access to clean water also contributes to poor hygiene and sanitation practices, further compounding the health problems of those East Sumba communities where Kawan Baik and Fair Future work so hard. Together, we are taking action to improve access to clean water sources, in these areas where no roads lead, to ensure the health and well-being of young children and their families. In addition to the physical hardship of fetching water, and as explained in this post, children in rural areas of East Sumba are often deprived of education and other opportunities because of this task. It is widespread (like in this picture of the day) that they miss school or other activities to help collect water, which affects their academic progress and social development.
Here people mainly only have access to contaminated water. This leads to many diseases, including gastrointestinal infections, skin diseases, parasitic diseases and other infectious diseases such as Malaria, Dengue Fever, Cholera, typhoid fever, hepatitis A or diarrhoea. Children and the elderly are particularly vulnerable to illnesses caused by contaminated water, a significant cause of infant mortality here.
In conclusion, ensuring access to clean water through a program like the #waterconnections project is our top priority that cannot be overlooked. Access to clean water is essential to sustaining life and maintaining good health for everyone here. Water plays a vital role in preventing the spread of the diseases mentioned above, ensuring people can lead healthier lives. Whether for drinking, cooking or cleaning, clean water is essential for everyday life. Without access, communities in the ultra-rural areas of East Sumba suffer from a lack of sanitation and hygiene, leading to various health problems.
Therefore, we must do everything we can to ensure that clean water is available to everyone who needs it.
Let’s prevent malaria rather than cure it!
In this "Picture of the Day" shows you three children from Kabanda Village in East Sumba (read this post here), where the PMC program is in place. In this village, very far from everything, especially health centres, malaria is very active and wreaking havoc. We are talking about 80% of children under 12 are affected. It is, therefore, essential to prevent and train families. This is what we are doing here.
The daily observations concerning the causes of malaria are multiple here. These include, in particular, the lack of access to health care, information on prevention methods, the unavailability of health centres and sanitation, and the growing resistance to antimalarial drugs for regions with access to these treatments.
A reminder for all Kawans: Malaria is transmitted by female mosquitoes of the "Genus Anopheles", throughout the East Sumba region. These mosquitoes breed in standing water, such as rainwater storage tanks and open water sources, most of the time in rural and deprived areas of East Sumba.
As Fair Future has repeatedly seen and repeated for years, the consequences of malaria are serious if nothing is done to treat it: High fever, severe headache, nausea and vomiting. If not treated quickly, the disease can progress and lead to severe complications, including kidney failure, anaemia, seizures and death.
It is essential to train families and rural communities to protect themselves from this disease to reduce its transmission. Also, by learning how to prevent and treat Malaria, rural families and communities will reduce the economic and social burden of the disease. Malaria entails high costs for families and communities, particularly medical expenses (if they can access them), school absenteeism, and reduced productivity.
As we apply it with the Primary Medical Care Program (PMC), training families and rural communities to protect themselves from malaria contributes to strengthening the resilience of these populations in the face of epidemics of infectious diseases such as HIV, Tuberculosis, Gastroenteritis, cholera etc…
Alexandre Wettstein from the Foundation’s Medico-Social Camp in East Sumba, Rumah Kambera, Lambanapu, on the 2nd of May 2023
Reduce health risks with clean water for families
In this "Picture of the Day" shows you what children do several times a day: Fetch water for the family with some 5-litre jerrycans. Most of the time, the young girls take care of this. Here in this photo, it is a young child of ten years. There are no daughters in the family. He does this job instead of going to school. He and his family have only two litres or less of water a day for eating, drinking, bathing and everything else.
Unfortunately, like here in Tana Mbanas (Sumba Tenggah), there is still a vast majority of villages in Sumba that do not have access to clean drinking water. In these villages, the inhabitants often depend on surface water sources such as rivers, lakes or ponds, which bacteria, viruses, chemicals or by animals and insects mostly contaminate.
The lack of clean water has severe consequences for the health of the inhabitants. Waterborne diseases, such as diarrhoea, cholera and typhoid, hepatitis A, Malaria and Dengue fever, are common where access to clean water and toilets is limited or absent. These diseases can be severe and even fatal, especially in children, pregnant women and the elderly.
To help villages without clean water in Sumba, Fair Future and Kawan Baik are implementing effective measures to improve access to clean and healthy water. Our solutions include drilling deep wells with our equipment, construction of water treatment plants, storage tanks, rainwater harvesting and storage, and installation of water management systems—irrigation and construction of healthy sanitation facilities.
We are still seeking funding and technical resources to set up sustainable, safe and clean water infrastructure in this region, one of the world's poorest and most dry.
Alexandre Wettstein from the Foundation’s Medico-Social Camp in East Sumba, Rumah Kambera, Lambanapu, on Mai 1st, 2023.
Fighting Malaria in Eastern Indonesia
East Sumba, where we work at the time of writing this article, was experiencing a dramatic malaria epidemic. In the first quarter of 2023, there were more than 28,000 cases of Malaria, a significant increase from the previous year. A few months ago, Fair Future declared this life-threatening emergency. Despite our best efforts, Malaria cases are increasing. Here, when a child has a fever, it is more than 80% of the time a question of Malaria. We conduct health education campaigns to raise awareness of the importance of malaria prevention and early detection. Efforts to control the epidemic should include the distribution of mosquito nets, the provision of essential antimalarial drugs, as well as rapid diagnostic tests.
Medical care for children affected by Malaria
In this "Picture of the Day", Fair Future and Kawan Baik medical teams provide medical care to a child most likely affected by Malaria. He is less than two years old and has a fever of 40.6. Her symptoms fit this diagnosis of Malaria. We give him appropriate primary medical care to reduce his fever as quickly as possible. Then he will go for treatment tomorrow at the nearest health centre, more than three hours from the village.
Malaria is a severe public health problem, especially in the ultra-rural and impoverished areas where Fair Future and Kawan Baik Foundations work so hard. Malaria is a life-threatening disease caused by the Plasmodium parasite is transmitted to humans through the bites of infected female Anopheles mosquitoes. Children under five and pregnant women are also particularly vulnerable to Malaria, as their immune systems are less developed and may have more difficulty fighting infection. People suffering from chronic illnesses are also vulnerable (HIV, Hepatitis, malnutrition, etc.)
Ultra-rural and poor areas such as East Sumba are particularly vulnerable to the spread of Malaria due to factors such as lack of water or contaminated water, deplorable housing conditions, lack of access to healthcare health and preventive measures, inadequate sanitation… Moreover, here we do not have antimalarial drugs nor rapid tests to detect the disease. This makes our treatment and prevention work very difficult.
PMC program evaluation in Lapinu
These women linked to the PMC program devote part of their lives to saving others. These unsung heroines work tirelessly to keep people from the danger of illness and injury. They put their lives on the line to ensure others can live to see another day. Teachers trained in primary medical care, these women are the backbone of these ultra-rural communities in East Sumba. They exemplify true bravery and selflessness, and we are eternally grateful for their service. Therefore, we express our deep gratitude to all women who save lives. Thanks for what you’re doing for the others.
PMC program evaluation in Kabanda
Kabanda is genuinely one of the most isolated I have ever seen. Getting it is difficult, even dangerous, at times. No road leads to this village; only extremely steep or steep stony paths allow us to go there. It took us over six hours to get there, including four hours of absolute terrain with the Truck of Life, a 4×4 medical truck specially designed for this journey. Kabanda is no exception; so many villages are in the same situation: That is to say, they have no road leading there. This raises – among other things – the question of access to health care, of course. And it is for these types of communities that Fair Future exists, and together with our friends from Kawan Baik, Sumba Volunteer and Charis Foundation, we have created this primary medical care program.
OUR 2025 IMPACT IN REMOTE VILLAGES
Medical consultations delivered in ultra-rural villages where no doctor, no clinic, and no alternative care exists.
Litres of safe water storage built or funded, helping families drink, cook, and wash without preventable disease.
People reached through daily health education on hygiene, malaria prevention, clean water, and basic nutrition.
Children who can now study, read, and move safely after dark thanks to clean, reliable solar light at home and school.
Annual Report 2024 – 17th Years of Concrete Action
Read Fair Future’s 2024 Annual Report, our concrete record of fieldwork in East Sumba: primary healthcare, clean water access, nutrition, and education. The 2025 Annual Report is currently being written and will be published within Q1 2026 (before March). For now, this link opens the full 2024 report in French and English.
→ Open the 2024 Annual Report
Essential Pages on Rural Health
Climate Change and Health
Climate change is not an abstract environmental issue. In ultra-rural communities, it directly worsens disease, water scarcity, malnutrition, and access to care. This page explains how climate impacts health long before emergencies appear.
Life Without Healthcare
In large parts of rural Indonesia, healthcare simply does not exist. No doctors, no clinics, no ambulances. This page explains what that absence means in real life, for children, families, and entire communities left alone with preventable diseases.
Keep in Touch via Instagram
Real moments from our medical, water, and community missions in ultra-rural Indonesia. Nothing staged — just the daily reality of our work on the ground.
Our core programmes in ultra rural Indonesia
We work in the extreme east of Indonesia, in ultra rural villages with no doctors, no electricity, and often no clean water. These programmes turn medical knowledge, community effort, and solidarity into concrete solutions for families who live far from any form of care.
Primary Medical Care
Trained Kawan Sehat health agents provide first line medical care in villages without doctors. With equipped medical backpacks and remote supervision, they treat wounds, infections, fevers, malaria, and chronic illness for 700 to 1 000 patients every month. This programme prevents simple problems from becoming emergencies.
Water Connections
We drill wells, build ferrocement reservoirs, and install safe water points so families can drink, cook, wash, and grow food without risking disease. Clean water reduces diarrhoea, malnutrition, and many infections we see daily in our clinics. Every tank and every tap is a public health intervention.
Kawan Against Malaria
In malaria endemic areas we combine prevention, rapid tests, treatment, and education. Long lasting insecticidal nets, indoor spraying, field studies, and posters help reduce fevers, anaemia, and deaths, especially among children and pregnant women. This programme links community action with rigorous medical follow up.