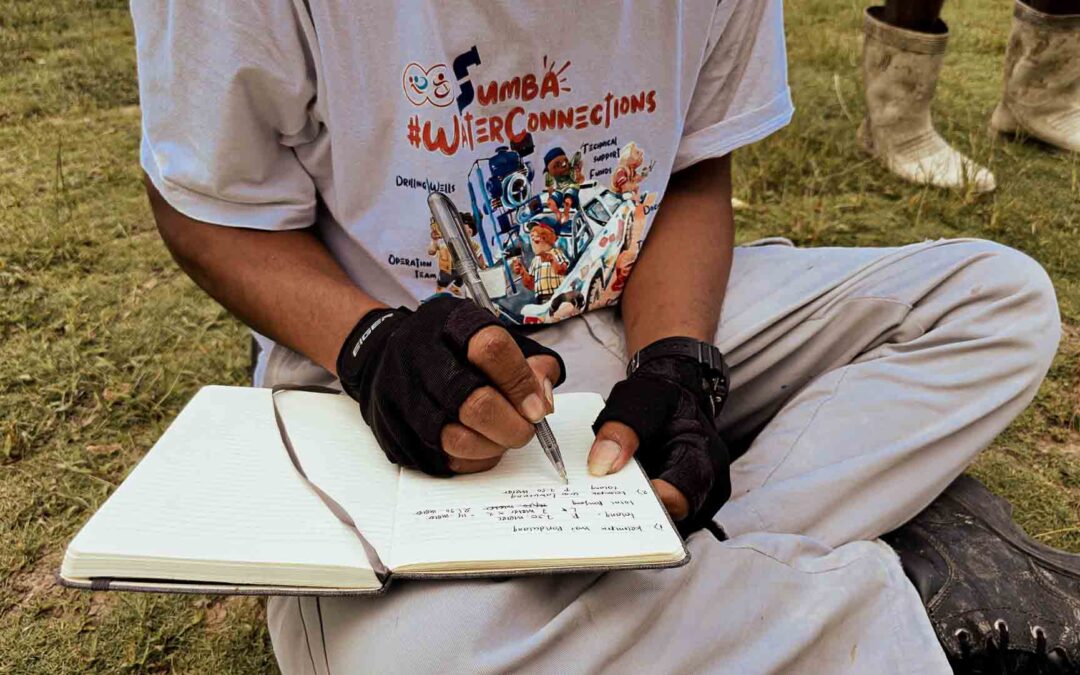
Kabanda is genuinely one of the most isolated I have ever seen. Getting it is difficult, even dangerous, at times. No road leads to this village; only extremely steep or steep stony paths allow us to go there. It took us over six hours to get there, including four hours of absolute terrain with the Truck of Life, a 4x4 medical truck specially designed for this journey. Kabanda is no exception; so many villages are in the same situation: That is to say, they have no road leading there. This raises - among other things - the question of access to health care, of course. And it is for these types of communities that Fair Future exists, and together with our friends from Kawan Baik, Sumba Volunteer and Charis Foundation, we have created this primary medical care program.
- Thank you for your interest.Two days in the village of Kabanda to assess the Primary Medical Care (PMC) program in one of Indonesia’s poorest, inaccessible and isolated villages.
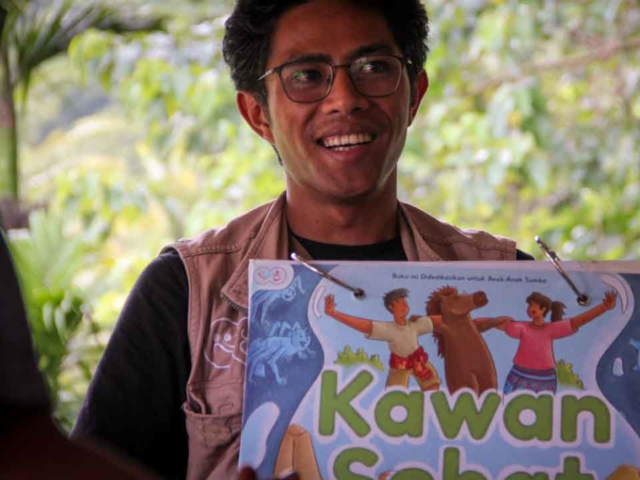
A vital and necessary medical program, which we introduced more than four months ago now, and which is a fundamental human success. Nearly 800 suffering people, children injured or suffering from malaria, have been cared for and treated successfully by the health workers we trained.
Hello everyone from Rumah Kambera, Sumba Timur,
As we presented in one of our last articles, the last week of March is the first week of April 2023; our teams went to five ultra-rural villages to evaluate the PMC (Primary Medical Care program) in favour of communities and villagers. During his visits, we also introduced the blood pressure monitoring program to people at risk of high blood pressure. You can read the article about it by clicking here on this link.
The five rural villages we visited for almost a week are among the most remote and isolated in the region and Indonesia. The five villages seen or revisited are Mbinudita, Mbatapuhu, Kabanda, Mahu and Lapinu. These are villages that are categorized as being “in pain”. That are places where people don’t eat and drink enough and can’t wash and care for themselves because they don’t have enough water. Here people live with less than 2 litres of water per person daily to do everything.
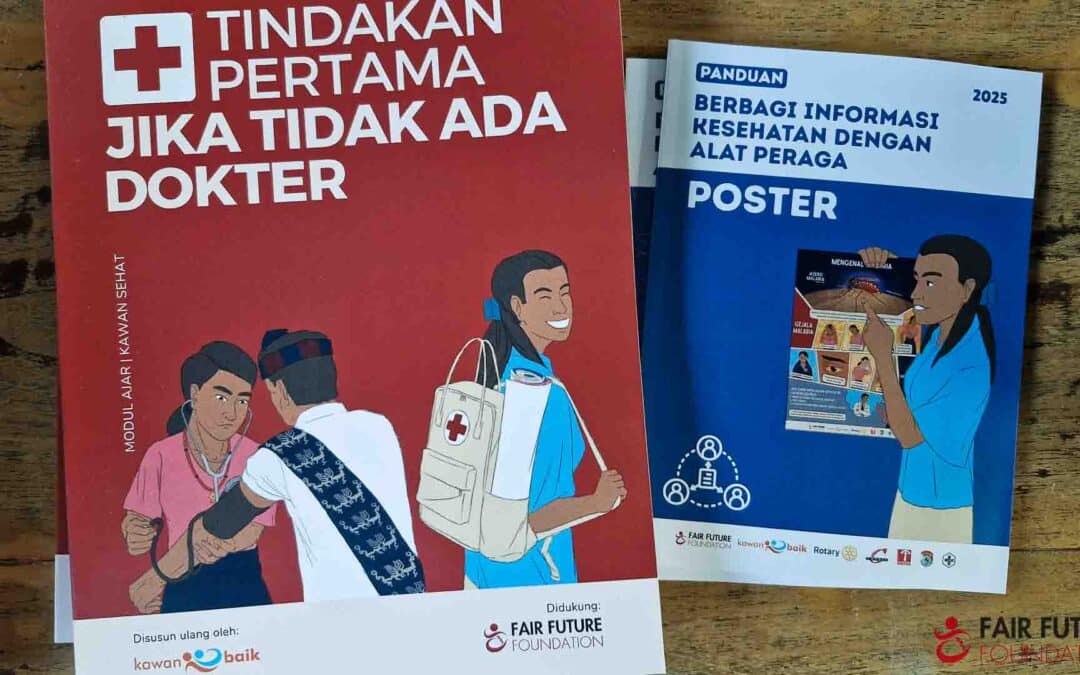
These villages lack access to electricity, water or direct medical care; we often discuss it. On average, the nearest health centre is more than three hours away from all dwelling houses with a motorized vehicle. For these few reasons in particular, we have introduced -with our medical friends and social partners- the primary medical care program for regions and populations from the ultra-rural areas in east Indonesia. As part of this article, we will show you and explain what we did in Kabanda:
Here, when a person is sick or injured when a woman has to give birth, one of the only ways for her to receive medical care is to carry her on the backs of people, and this for several hours, even an entire day, to the nearest healthcare centre. This person is also unsure about arriving at the care centre, called “Puskesmas or Pustu”.
We will tell you an example of life in these villages isolated from everything, including medical care centres:
This story happened about a fortnight ago in a tiny village near Kabanda. A woman living in one of the houses here was pregnant with her first child. This woman was over eight months pregnant when suddenly, she no longer felt any fetus movement in her womb. Panicked, she and her husband visited the nearest medical centre (Puskesmas). From these houses and these villages, there is no good path and, of course, no road. Families very rarely have a scooter and no car. Therefore, several people decided to transport this suffering woman, seized with terrible abdominal pain, to the nearest Puskesmas. Reaching this health centre usually takes three to four hours of walking. This medical event happened at the end of the day; it was already dark and raining hard. The paths were very steep, so the water ran down them hard, making them slippery. Standing, walking, and moving around while carrying a suffering person at arm’s length was tricky. And we still had to cross three rivers whose current had increased because of the falling rain.
After almost eight hours of walking, this woman and the people who carried her could reach the small Mahu health centre; her baby had died. She suffered from significant medical complications during the trip, deteriorating her health.
This is what life can be like for people with medical conditions who don’t have access to direct medical or healthcare. For example, we have hundreds of those related to illnesses, injuries, malaria, Dengue fever, asthma attacks, bites, or burns. Most of the time, these needy people cannot get to a care centre in time. They will stay home and (maybe) self-medicate.
Three young women, three teachers, three Kawan Sehat agents, and three people who save lives. Three superheroines! Their names are Merlin, Siyane and Sarlota.
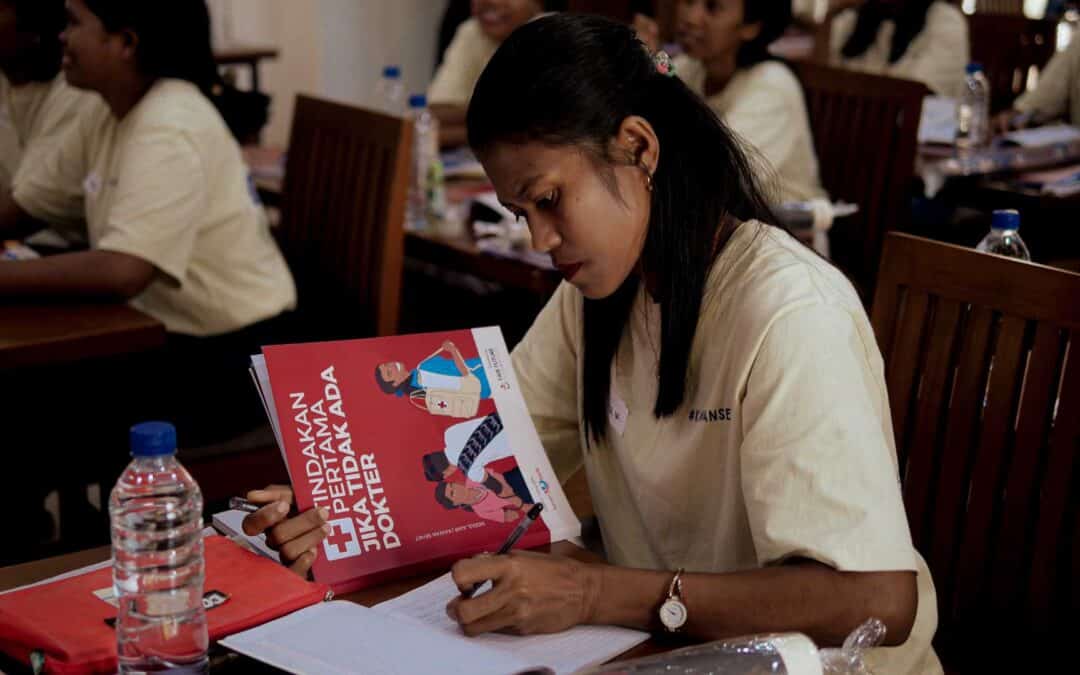
In the company of the three health workers “Kawan Sehat” of this village, we lived a day (in fact, two days) more than extraordinary. These three women? It’s just three superheroes! They told us how they had experienced all this care for young and sick patients, injured or ill children, feverish or suffering from Malaria, and how they had reacted, treated, and cared for them.
Merlin, Siyane and Sarlota also asked us how this drug works, how to treat this or that problem, and the best behaviour to adapt to a patient with X symptoms. They also told us of their great pride in that of three women between the ages of 25 and 30 who suddenly took on responsibilities and importance in their village.
In principle, here, and related to local culture and traditions, a woman takes care of household chores, fetching water, cooking for the children, and caring for the family. These three female superheroes are not only teachers within the framework of Charis Sumba, but they are also now – and for more than four months – the health workers of the PMC program. They are the ones who can save a life in the absence of a medical centre, medical care or a doctor in the village. This is not anything in terms of enhancing the role of women in ultra-rural villages; this is immense and important progress.
And as we did in the village of Mbinudita and Mabatapuhu, we gave new prerogatives to these two Kawan Sehat Agents: Since April, here in this village of Kabanda, Merlin, Siyane and Sarlota can measure the blood pressure of a patient, and in case of hypertension, to give appropriate medical treatment. It is a social and medical revolution, in our opinion. You can read much more about this program here too.
Alexandre Wettstein from the Foundation’s Medico-Social Camp in East Sumba, Rumah Kambera, Lambanapu, on April 20th, 2023.
Kabanda, PMD program evaluation, medical care and training of health workers
Two days in the village of Kabanda to assess the primary medical care program in one of Indonesia’s poorest, inaccessible and isolated villages.
A vital and necessary medical program, which we introduced more than four months ago now, and which is a fundamental human success. Nearly 800 suffering people, children injured or suffering from malaria, have been cared for and treated successfully by the health workers we trained.
Hello everyone from Rumah Kambera, Sumba Timur,
As we presented in one of our last articles, the last week of March is the first week of April 2023; our teams went to five ultra-rural villages to evaluate the PMC (Primary Medical Care program) in favour of communities and villagers. During his visits, we also introduced the blood pressure monitoring program to people at risk of high blood pressure. You can read the article about it by clicking here on this link.
The five rural villages we visited for almost a week are among the most remote and isolated in the region and Indonesia. The five villages seen or revisited are Mbinudita, Mbatapuhu, Kabanda, Mahu and Lapinu. These are villages that are categorized as being “in pain”. That are places where people don’t eat and drink enough and can’t wash and care for themselves because they don’t have enough water. Here people live with less than 2 litres of water per person daily to do everything.
These villages lack access to electricity, water or direct medical care; we often discuss it. On average, the nearest health centre is more than three hours away from all dwelling houses with a motorized vehicle. For these few reasons in particular, we have introduced -with our medical friends and social partners- the primary medical care program for regions and populations from the ultra-rural areas in east Indonesia. As part of this article, we will show you and explain what we did in Kabanda:
Kabanda is genuinely one of the most isolated I have ever seen. Getting it is difficult, even dangerous, at times. No road leads to this village; only extremely steep or steep stony paths allow us to go there. It took us over six hours to get there, including four hours of absolute terrain with the Truck of Life, a 4×4 medical truck specially designed for this journey. Kabanda is no exception; so many villages are in the same situation: That is to say, they have no road leading there. This raises – among other things – the question of access to health care, of course. And it is for these types of communities that Fair Future exists, and together with our friends from Kawan Baik, Sumba Volunteer and Charis Foundation, we have created this primary medical care program.
Here, when a person is sick or injured when a woman has to give birth, one of the only ways for her to receive medical care is to carry her on the backs of people, and this for several hours, even an entire day, to the nearest healthcare centre. This person is also unsure about arriving at the care centre, called “Puskesmas or Pustu”.
We will tell you an example of life in these villages isolated from everything, including medical care centres:
This story happened about a fortnight ago in a tiny village near Kabanda. A woman living in one of the houses here was pregnant with her first child. This woman was over eight months pregnant when suddenly, she no longer felt any fetus movement in her womb. Panicked, she and her husband visited the nearest medical centre (Puskesmas). From these houses and these villages, there is no good path and, of course, no road. Families very rarely have a scooter and no car. Therefore, several people decided to transport this suffering woman, seized with terrible abdominal pain, to the nearest Puskesmas. Reaching this health centre usually takes three to four hours of walking. This medical event happened at the end of the day; it was already dark and raining hard. The paths were very steep, so the water ran down them hard, making them slippery. Standing, walking, and moving around while carrying a suffering person at arm’s length was tricky. And we still had to cross three rivers whose current had increased because of the falling rain.
After almost eight hours of walking, this woman and the people who carried her could reach the small Mahu health centre; her baby had died. She suffered from significant medical complications during the trip, deteriorating her health.
This is what life can be like for people with medical conditions who don’t have access to direct medical or healthcare. For example, we have hundreds of those related to illnesses, injuries, malaria, Dengue fever, asthma attacks, bites, or burns. Most of the time, these needy people cannot get to a care centre in time. They will stay home and (maybe) self-medicate.
Three young women, three teachers, three Kawan Sehat agents, and three people who save lives. Three superheroines! Their names are Merlin, Siyane and Sarlota.
In the company of the three health workers “Kawan Sehat” of this village, we lived a day (in fact, two days) more than extraordinary. These three women? It’s just three superheroes! They told us how they had experienced all this care for young and sick patients, injured or ill children, feverish or suffering from Malaria, and how they had reacted, treated, and cared for them.
Merlin, Siyane and Sarlota also asked us how this drug works, how to treat this or that problem, and the best behaviour to adapt to a patient with X symptoms. They also told us of their great pride in that of three women between the ages of 25 and 30 who suddenly took on responsibilities and importance in their village.
In principle, here, and related to local culture and traditions, a woman takes care of household chores, fetching water, cooking for the children, and caring for the family. These three female superheroes are not only teachers within the framework of Charis Sumba, but they are also now – and for more than four months – the health workers of the PMC program. They are the ones who can save a life in the absence of a medical centre, medical care or a doctor in the village. This is not anything in terms of enhancing the role of women in ultra-rural villages; this is immense and important progress.
And as we did in the village of Mbinudita and Mabatapuhu, we gave new prerogatives to these two Kawan Sehat Agents: Since April, here in this village of Kabanda, Merlin, Siyane and Sarlota can measure the blood pressure of a patient, and in case of hypertension, to give appropriate medical treatment. It is a social and medical revolution, in our opinion. You can read much more about this program here too.
Alexandre Wettstein from the Foundation’s Medico-Social Camp in East Sumba, Rumah Kambera, Lambanapu, on April 20th, 2023.