The last week of March is the first week of April 2023; our teams travelled to five ultra-rural villages to assess the Primary Medical Care Program (PMC) for communities and villagers.
During the first three months of the exercise, several hundred cases were treated by the health workers of the direct medical care programme. As a reminder, there are more than sixty women health workers.
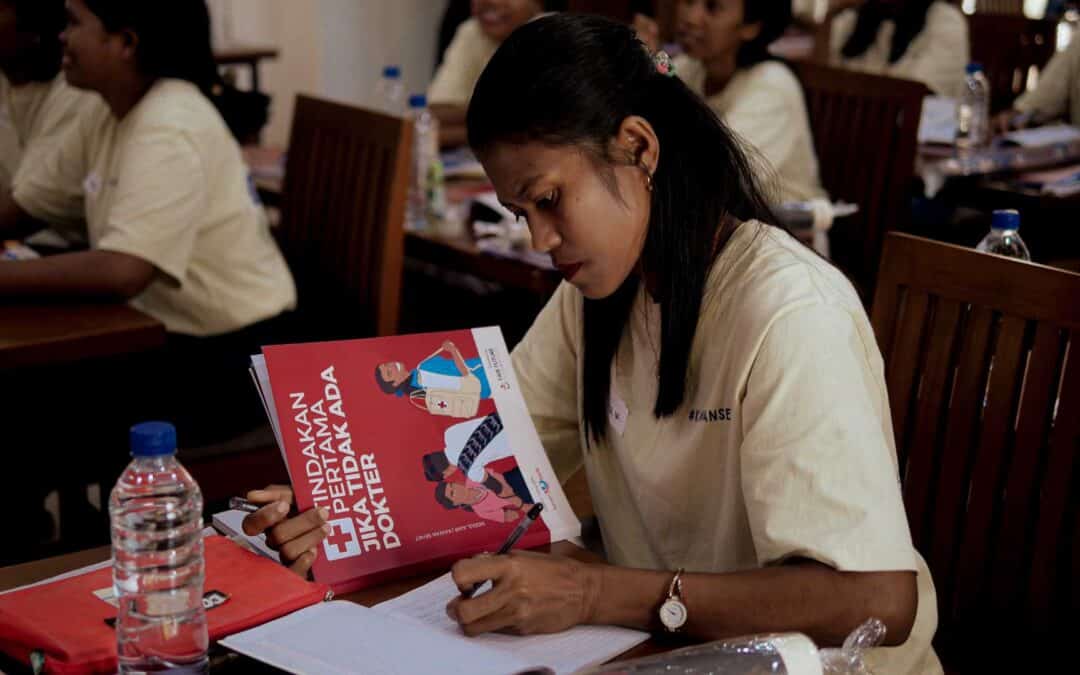
These “Kawan Sehat” health workers are first and foremost teachers who teach in their small schools, in their villages isolated from everything and most of the time where no road leads. They were all born where they worked, were raised, and lived with their families. To be able to teach, they all received a three-month training course given by our friends at the Charis Foundation.
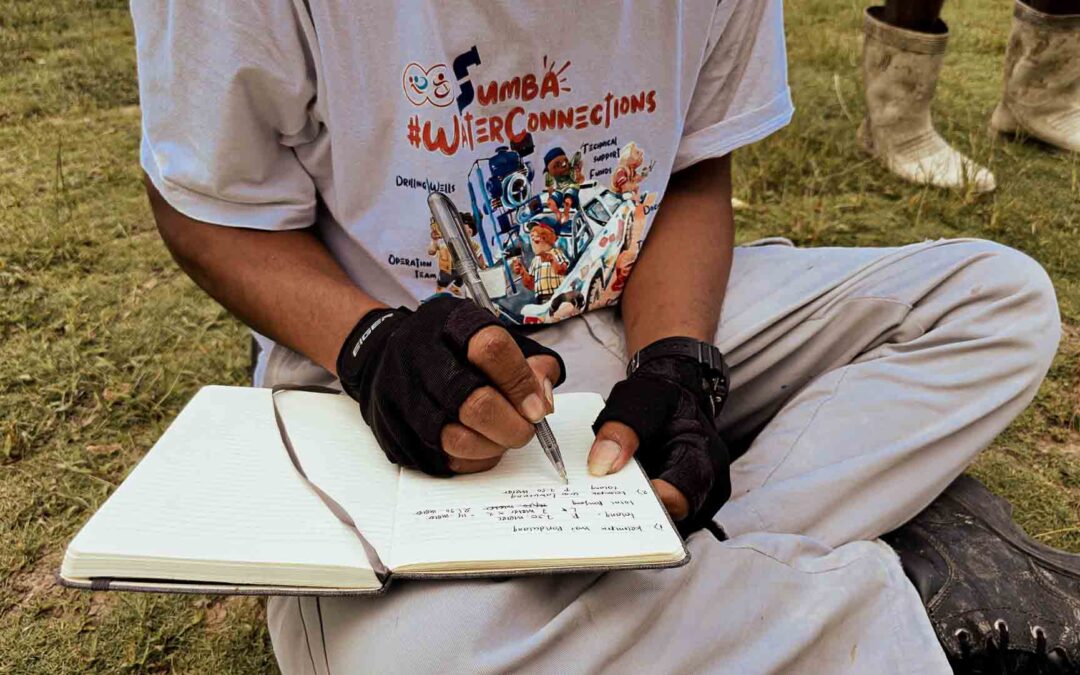
The five rural villages we visited for almost a week are among the most remote and isolated in the region and Indonesia. Accessing it is incredibly complicated and challenging, as the roads are impassable, steep and dangerous. A typical vehicle cannot access these villages; you must have a well-equipped 4×4 or a trail or enduro motorcycle. We went there with the help of three cars and ten people, including members of the foundation’s medical and social team.
The five villages visited or revisited are Mbinudita, Mbatapuhu, Kabanda, Mahu and Lapinu. Not all these villages can access electricity, water or direct medical care. On average, the nearest health centre is more than three hours away from all dwelling houses with a motorized vehicle. When a person is sick and injured and needs treatment, one of the only ways is to transport them on people’s backs, for several hours, or even a whole day, to the “nearest” care centre.
As part of this article, we show and explain what we did in Mbatapuhu.
After the evaluation and training day in Mbinudita, we left by road to join Mbatapuhu. It took us about five hours to travel the twenty kilometres that separated these two villages. The last fifteen kilometres were pure off-road: In the mud, in the stones, on narrow, steep and highly hilly paths. Often our vehicles are put to slide near the ravine, but everything went well.
We arrived around 8 p.m. in the village of Mbatapuhu, a little tired from the previous days. A prominent religious ceremony was concentrated in one of the wooden and bamboo houses in the town. A hundred people, including most men, wore traditional clothes, were gathered there, smoking and drinking. We were invited to share a moment with them and to enter the house where the religious ceremony was taking place. We talked a lot, learned, and exchanged on the problems of their everyday life. How difficult it is to live here.
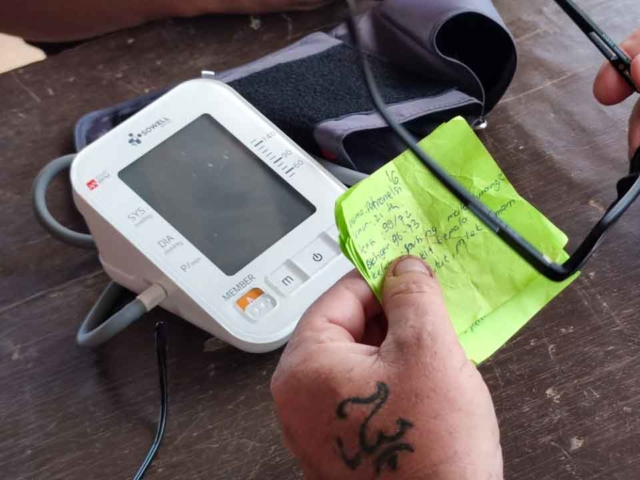
Our team spent the night in the vehicles or the village church for a short night, just a few hours of sleep. We knew we would be swamped in the morning with the primary medical care program and its local evaluation. But also the training of the two Kawan Sehat agents in using a tensiometer to measure the blood pressure of the inhabitants of their village.
Archer and Mensi are two young women in their thirties, teachers in this village. They are also the health workers of the Primary Medical Care Programme; we call them the “Kawan Sehat” workers, the healthy friends. During the first months of the program, these two people treated approximately 80 people, the majority of whom were children. That is to say that more than 80 people did not have to go to the nearest hospital or health centre and therefore spent several hours on the road.
This also means that, for example, when a child was injured, Acher and Mensi knew and could provide the appropriate medical care, thus avoiding infection or medical complications. I like to say, and it is a fact for all of us, that thanks to their heroism, talent and enthusiasm, these more than 60 people who make up the health workers of the PMC program save lives.
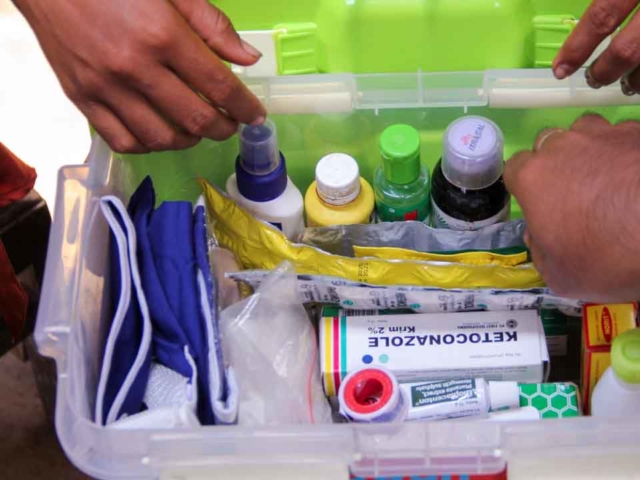
We went through most of the cases they had to deal with and answered many of their questions, such as how to give a specific medicine or treat a wound or a burn. We have also supplemented their medical equipment stocks with new drugs and digital thermometers to measure children’s temperature because malaria is rampant here.
And as we did in the village of Mbinudita (ref read this article here), we gave new prerogatives to these two Kawan Sehat Agent: Since April here in this village of Mbatapuhu, Acher and Mensi can measure the blood pressure of a patient, and in case of hypertension, to give appropriate medical treatment. It is a social and medical revolution, in our opinion.
The fight and prevention of cardiovascular diseases are significant here in ultra-rural regions. This, for example, led us to talk about active and passive smoking. Make people understand that tobacco is dangerous for your health and that it is also the cause of high blood pressure and, consequently, strokes, heart attacks, respiratory problems, and a multitude of other tobacco-related diseases. You can read much more about this program here too.
Alexandre Wettstein from the Foundation’s Medico-Social Camp in East Sumba, Rumah Kambera, Lambanapu, on April 12th, 2023.
Mbatapuhu, PMD program evaluation, medical care and training of health workers
The last week of March is the first week of April 2023; our teams travelled to five ultra-rural villages to assess the Primary Medical Care Program (PMC) for communities and villagers.
During the first three months of the exercise, several hundred cases were treated by the health workers of the direct medical care programme. As a reminder, there are more than sixty women health workers.
These “Kawan Sehat” health workers are first and foremost teachers who teach in their small schools, in their villages isolated from everything and most of the time where no road leads. They were all born where they worked, were raised, and lived with their families. To be able to teach, they all received a three-month training course given by our friends at the Charis Foundation.
The five rural villages we visited for almost a week are among the most remote and isolated in the region and Indonesia. Accessing it is incredibly complicated and challenging, as the roads are impassable, steep and dangerous. A typical vehicle cannot access these villages; you must have a well-equipped 4×4 or a trail or enduro motorcycle. We went there with the help of three cars and ten people, including members of the foundation’s medical and social team.
The five villages visited or revisited are Mbinudita, Mbatapuhu, Kabanda, Mahu and Lapinu. Not all these villages can access electricity, water or direct medical care. On average, the nearest health centre is more than three hours away from all dwelling houses with a motorized vehicle. When a person is sick and injured and needs treatment, one of the only ways is to transport them on people’s backs, for several hours, or even a whole day, to the “nearest” care centre.
As part of this article, we show and explain what we did in Mbatapuhu.
After the evaluation and training day in Mbinudita, we left by road to join Mbatapuhu. It took us about five hours to travel the twenty kilometres that separated these two villages. The last fifteen kilometres were pure off-road: In the mud, in the stones, on narrow, steep and highly hilly paths. Often our vehicles are put to slide near the ravine, but everything went well.
We arrived around 8 p.m. in the village of Mbatapuhu, a little tired from the previous days. A prominent religious ceremony was concentrated in one of the wooden and bamboo houses in the town. A hundred people, including most men, wore traditional clothes, were gathered there, smoking and drinking. We were invited to share a moment with them and to enter the house where the religious ceremony was taking place. We talked a lot, learned, and exchanged on the problems of their everyday life. How difficult it is to live here.
Our team spent the night in the vehicles or the village church for a short night, just a few hours of sleep. We knew we would be swamped in the morning with the primary medical care program and its local evaluation. But also the training of the two Kawan Sehat agents in using a tensiometer to measure the blood pressure of the inhabitants of their village.
Archer and Mensi are two young women in their thirties, teachers in this village. They are also the health workers of the Primary Medical Care Programme; we call them the “Kawan Sehat” workers, the healthy friends. During the first months of the program, these two people treated approximately 80 people, the majority of whom were children. That is to say that more than 80 people did not have to go to the nearest hospital or health centre and therefore spent several hours on the road.
This also means that, for example, when a child was injured, Acher and Mensi knew and could provide the appropriate medical care, thus avoiding infection or medical complications. I like to say, and it is a fact for all of us, that thanks to their heroism, talent and enthusiasm, these more than 60 people who make up the health workers of the PMC program save lives.
We went through most of the cases they had to deal with and answered many of their questions, such as how to give a specific medicine or treat a wound or a burn. We have also supplemented their medical equipment stocks with new drugs and digital thermometers to measure children’s temperature because malaria is rampant here.
And as we did in the village of Mbinudita (ref read this article here), we gave new prerogatives to these two Kawan Sehat Agent: Since April here in this village of Mbatapuhu, Acher and Mensi can measure the blood pressure of a patient, and in case of hypertension, to give appropriate medical treatment. It is a social and medical revolution, in our opinion. The fight and prevention of cardiovascular diseases are significant here in ultra-rural regions. This, for example, led us to talk about active and passive smoking. Make people understand that tobacco is dangerous for your health and that it is also the cause of high blood pressure and, consequently, strokes, heart attacks, respiratory problems, and a multitude of other tobacco-related diseases.